Day 2 :
Keynote Forum
Zhen Su
Wenzhou Medical University, China
Keynote: Risk factors of progressive IgA nephropathy which progress to end stage renal disease within ten years
Time : 10:00-10:45

Biography:
Su Zhen has completed her MD from Wenzhou Medical University; PhD from Second Military Medical University and; Post-doctoral studies from Emory University School of Medicine. She is the Vice-Director of Renal Division at First Affiliated Hospital of Wenzhou Medical University. She has published more than 40 papers in reputed journals and had oral presentation in ASN 2005 (American Society of Nephrology) meeting and WCN 2007 (ISN World Congress of Nephrology) meeting.
Abstract:
Background & Aim: There were few related studies aiming to severe IgA nephropathy (IgAN) which could progress rapidly to end stage renal disease (ESRD) within ten years. To find valuable clinical or pathological factors and promising precautions is essential.
Method: A single center case-control study was performed. 50 ESRD patients with the primary cause of IgAN and a short renal survival time of less than ten years after diagnose were enrolled in the case group. 100 IgAN patients with a renal survival time of more than ten years were enrolled in the control group. IgA Oxford classification scores, clinical data at baseline and during the follow-up were collected. Multivariate logistic regression was used to investigate factors associated with the development of ESRD.
Results: There were significant differences in baseline clinical data between these two groups, as well as the constituent ratio of Oxford MEST-score. Distinct differences were observed in time-average uric acid (TA-UA), time-average hemoglobin (TA-Hb), time-average albumin (TA-Alb), time-average total cholesterol (TA-TC) and time-average urinary protein (TA-P) during the follow-up. In multivariate logistic models, IgA oxford score M1 (OR=5.10, P=0.018) and eGFR (OR=0.97, P=0.039) at biopsy, TA-UA (OR=2.06, P=0.026) and TA-Hb (OR=0.53, P=0.022) during the follow-up were identified independent factors for developing ESRD.
Conclusion: IgAN patients with pathological assessment of M1, low baseline eGFR, TA-Hb and high TA-UA were more likely to progress to ESRD, and should be paid more attention. Appropriate regulations of UA, Hb and urine protein after diagnose may be a promising treatment.
Keynote Forum
Surjit Tarafdar
Western Sydney University, Australia
Keynote: Atypical familial hyperaldosteronism in a family
Time : 10:45-11:30

Biography:
Surjit Tarafdar is a Nephrologist working at Blacktown Hospital in Sydney since 2014 and has additional position of Conjoint Lecturer at Western Sydney University Medical School since March 2014. He had conceptualized and eventually co-written “Passing the FRACP Written Examination-Questions and Answers” published by Wiley-Blackwell in 2013. He has started the annual “Revise Nephrology”, a weekend nephrology refresher programme for trainees with the aim of helping them to understand nephrology better and pass the FRACP theory examination. In 2017, 182 doctors attended Revise Nephrology. He is currently editing a nephrology book entitled “Lecture Notes in Nephrology” which is due to be published by Wiley-Blackwell publishing house in April 2018.
Abstract:
Defect of CYP11B1, or 11-beta-hydroxylase 1(11β-OH 1) deficiency causes 5% of congenital adrenal hyperplasia (CAH). A 27-year-old male with history of hypertension from the age of 21 and non-compliance was found to have hypokalaemia with metabolic alkalosis. Investigations revealed he had primary aldosteronism with an aldosterone/renin ratio of more than 200 (normal <30). CT imaging of the adrenal glands showed hyperplastic right adrenal gland. Given the young age and strong family history of early onset hypertension patient had genetic tests which revealed a large deletion in CYP11B1. No evidence of hyperandrogenism was found. Subsequently patient’s 52 year old father who had been hypertensive since his twenties was investigated and found to have primary hyperaldosteronism with the same genetic defect. Both father and son responded very well to spironolactone. 11β-OH1 associated CAH is characterized by hyperandrogenism along with accumulation of 11-deoxycortisol and 11-deoxycorticosterone. 11-deoxycorticosterone (which has intrinsic mineralocorticoid activity) causes hypokalemic hypertension and suppressed aldosterone production. However, our patient family has a significantly elevated aldosterone to renin ratio suggesting that blockage of the cortisol pathway caused activation of the mineralocorticoid pathway rather than the androgen pathway. This is the first documented case of a deletion in gene CYP11B1 presenting with hypertension and primary aldosteronism rather than hyperandrogenism and hypertension with hypoaldosteronism. This group of patients should be recognized as a new subset of familial hyperaldosteronism rather than CAH.
- Chronic Kidney Disease | Kidney Cancer | Hypertensive Associated Kidney Diseases | Dialysis | Urinary Tract Infections |
Location: Olimpica 3 + 4

Chair
Vladimirs Strazdins
Medical Society Gailezers, Ltd., Latvia

Co-Chair
Nadica Ristoska-Bojkovska
KB Acibadem Sistina, Republic of Macedonia
Session Introduction
Banan Abbas Mustafa Osman
Bristol Urological Institute, UK
Title: Medical expulsive therapy for ureteric stones: Analysing the evidence from systematic reviews and meta-analysis of powered double-blinded randomised controlled trials

Biography:
Banan Abbas Mustafa Osman is a British urology trainee joined University of Medical Science and Technology. She is an Honorary Clinical Tutor for the Severn School of Surgery. She is also a teaching faculty member at Royal College of Surgeons England. She was appointed annually over three years as a Surgical and Urology trainee representative in Junior’s Doctor’s Forum in the Royal Marsden NHS Foundation Trust & North Bristol NHS Trust. She was a Clinical Investigator in VORTEX Clinical Trial. She held a position of Assistant Director of training in SMA International Training School.
Abstract:
Urinary tract stones affect 1–15% of the general population and the incidence is on the rise. Annual costs for stone disease have rapidly increased over the years and most patients with ureteral colic or other symptoms seek medical care. This has led to a plethora of research into the field aiming at finding a medication that will increase stone passage, shorten time to passage, and alleviate pain. The role of medical expulsive therapy (MET) is debatable with studies showing benefit for medical expulsive therapy (MET), whilst others reported no benefit. However, despite the multitude of trials published, the debate remains, as most of the research is riddled with bias and confounding factors. We therefore conducted a Cochrane style systematic review and a pooled meta-analysis on published literature from 1990 to 2016, to include low risk of bias (RoB) randomised controlled trials (RCTs) and a power calculation to investigate the efficacy and safety of medical expulsive therapy (MET). Pooled analysis of powered RCTs with low RoB would suggest, MET with the use of an a-blocker does increase stone expulsion rates (a-blockers 78% vs. 71% control) (P<0.001). Furthermore, their role is more significant for larger (>5 mm) stones (a-blockers 75% vs. 61% control) (P=0.02) and stones in the lower ureter (a-blockers 83% vs. 72% control) (P<0.001). However, MET was associated with side-effects, albeit not severe.
Vladimirs Strazdins
Medical Society Gailezers, Ltd., Latvia
Title: Recurrent urinary tract Infections in adults in Latvia: Additional findings from 2014 study

Biography:
Vladimirs Strazdins completed his Graduation from Riga Stradins University in 1977 and dedicated his further carrier to nephrology and pediatric nephrology. From 1992 till 2009, he worked as a Head of Nephrology at University Hospital for Children in Riga. From 2004 till 2012, he was a member of European Pediatric Dialysis working group, participating in creation of European guidelines on the subject. In 1999, he was awarded with Special Recognition Award for developing the pediatric ESRD treatment program in Latvia and Lithuania; in 2013 awarded with Honor Medal Tempus Hominis 2nd degree for outstanding achievements in medicine.
Abstract:
Antimicrobial resistance is a growing worldwide problem. Urinary tract infection (UTI) is not an exception. Furthermore, the recent trends may prohibit the further use of fluoroquinolones in UTI treatment. Therefore, it is crucial to regularly update the bacterial flora spectrum data and the efficacy of the recommended empiric treatment to make timely and appropriate amendments where necessary. This observational study was comprised in July-November 2014, when family physicians across Latvia submitted the anonymous patient data on recurrent UTI treatment in their practice. Bacterial flora spectrum in Latvian adult recurrent UTI population was fairly consistent with data from other European countries, with prevalent Escherichia coli cultures. The soluble nitrofuran derivate (NFD) - in Latvia Furamags ® in particular was clinically effective in all patients, even in culture-negative or NFD-resistant patients. There was not a single case without any improvement in controlled parameters – Furamags ® was clinically effective in all cases, including pyelonephritis. This confirms unique multifactorial antibacterial activities of NFDs, which simultaneously inhibit protein synthesis, aerobic energy metabolism, DNA synthesis, RNA synthesis and cell-wall synthesis, thus ensuring antibacterial activity even against the seemingly resistant flora. The current first-choice empiric treatment of recurrent UTI by NFDs may stay unchanged. Particular NFD used in Latvia (Furamags ®) is safe, well-tolerated and effective first-line UTI (including pyelonephritis) treatment choice.
Nadica Ristoska-Bojkovska
Clinical Hospital Acibadem-Sistina, Macedonia
Title: Congenital anomalies of the kidneys and urinary tract

Biography:
Nadica Ristoska-Bojkovska has completed Faculty of Medicine Specialist in Pediatrics; Subspecialist in Nephrology Faculty of Medicine in 1989 at Saints Cyril and Methodius University of Skopje, Skopje and she was employed at University Children's Hospital in Skopje 1990. She works at Clinical Hospital Acibadem-Sistina in Skopje from 2015. She started Pediatric specialization and passed the final specialization exam in 1996. She completed her Master Degree thesis in 2004 and; PhD in 2015 at Saints Cyril and Methodius University of Skopje, Skopje. She published many papers of scientific work and had fellowship at Charite Hospital, Berlin; Children's Hospital in Hanover and; Max-Dellbruck Center for Molecular Medicine in Berlin-Buch.
Abstract:
Congenital anomalies of the kidneys and urinary tract (CAKUT) are found in 3-6 out of 1000 of the newborns or according to some statistics they are represented in 0.5% of all pregnancies. Congenital abnormalities of the kidneys and urinary tract present a family of diseases of various anatomic spectrums, including renal anomalies, and anomalies of the bladder and urethra. This paper is motivated from the awareness that so far in Macedonia there has been no major or serious study prepared in relation to congenital kidney and urinary tract anomalies. The study was retrospective – prospective which means that it included newly diagnosed patients suffering from CAKUT, as well as those patients with already diagnosed and well defined CAKUT on the basis of imaging studies which have been processed according to the protocol for this study. A series of 749 pediatric patients with diagnosed congenital anomaly of the kidneys and urinary tract (CAKUT) has been analyzed at the Pediatric Clinic in the period from 2010 until 2015. In 25% CAKUT has been detected by prenatal ultrasound screening. The molecular diagnosis of patients with renal hypo dysplasia and renal agenesis can be achieved with copy number variation analysis in 10% of the patients. With this study we created a database of patients with syndromic and non-syndromic CAKUT, identified an unambiguous existence of the genetic factor through the familial ultrasound screening and existence of extra-renal abnormalities, thus enabling participation in future multicentric studies.
Hassan Kamal
Galilee Medical Center, Israel
Title: The impact of peritoneal glucose load on blood pressure in peritoneal dialysis patients

Biography:
Kamal Hassan is a specialist in Internal Medicine, Nephrology and Hypertension. He is Head of Peritoneal Dialysis Unit and In-patient Nephrology and Hypertension Department in the Galilee Medical Center, Naharyia, Israel. Also he is Clinical lecturer Faculty of Medicine. Main research interest: peritoneal dialysis and clinical nephrology.
Abstract:
Background: Hypertension is considered well-known independent risk factors for cardiovascular morbidity and mortality in peritoneal dialysis (PD) patients. Cardiovascular complications are the main cause of morbidity and mortality in patients with end-stage renal disease and dialysis patients. Peritoneal glucose load (PGL) contributes to the development of cumulative peritoneal membrane damage and increased permeability, leading to fluid accumulation and elevated blood pressure.
The effects of PGL on hydration status, systemic inflammation, left ventricular mass, depression and male sexual dysfunction among PD patients was evaluated in our peritoneal unit in several prospective cross sectional studies conducted in the last 5 years (2014-2018).The relationship between PGL and blood pressure was not investigated before. Based on the data obtained from the mentioned studies and additional data that received from the usual maintenance follow up visits we evaluated retrospectively the influence of PGL on blood pressure in patients on maintenance PD.
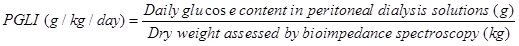
Methods: Office blood pressure measurements were used. If white coat hypertension is suspected, a 24 hour blood pressure study was performed to assess the patient's overall blood pressure profile using Mobil-O-Graph device for 24-hour ambulatory blood pressure monitoring (Manufacture: Industrielle Entwicklung Medizintechnik GmbH, D-52222 Stolberg, Germany). The hydration status was assessed by a whole-body bioimpedance technique (BIS) using a Fresenius Medical Care Body Composition Monitor (BCM) device (Fresenius Medical Care, Bad Homburg, Germany). The PGL was assessed by PGL index (PGLI), which refers to the net glucose content (monohydrated or unhydrated) (g) in the PD solutions administered in the daily PD prescription divided by the dry body weight (kg) assessed by BIS:
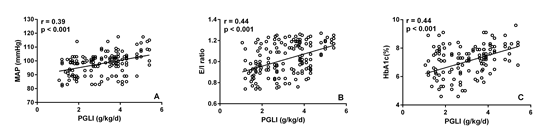
Results: One hundred fifty nine medical records of stable PD patients were evaluated retrospectively. Significant positive correlations were found between PGLI and mean arterial preasure (MAP), extracellular water (ECW)/ intracellular water (ICW) ratio and HbA1c. MAP, ECW/ ICW ratio and HbA1c were significantly higher in patients with PGLI > 3g/kg/day compared with those with PGLI ≤ 3g/kg/day.
Conclusions: PGL may be associated with higher blood pressure, overhydration and poor glycaemic control in PD patients. PGLI could be applied in managing PD patients as a practical tool for the quantitative assessment of the PGL. PGLI values bellow 3 g/kg/day should be targeted.
|
p |
Patients with PGLI > 3 g/kg/day n=76 |
Patients with PGLI > 3 g/kg/day n=83 |
|
|
<0.001 |
95.3±6.8 |
100.4±7.9 |
MAP (mmHg) |
|
<0.001 |
0.964±0.144 |
1.072±0.136 |
E/I ratio |
|
<0.001 |
6.56±1.13 |
7.52±0.94 |
HbA1c (%) |
Pai-Yen Pan
Chang Gung Memorial Hospital, Taiwan
Title: Mixed epithelial stromal tumor of the kidney: The male case and literature review

Biography:
Pai-Yen Pan has completed his MD degree at the age of 28 from Chang Gung University of Medicine. He is the resident doctor in the division of urology, department of surgery, Chang Gung Memorial Hospital. He has published a case report.
Abstract:
Mixed epithelial stromal tumor of the kidney (MESTK) is a rare genitourinary tract tumor. It was first presented by Michal and Syrucek in 1998.1 This tumor is characterized by its composition of both stromal solid areas and epithelial elements. Previous reports showed that MESTK attacks mostly middle-aged peri-menopausal women with estrogen therapy history, which indicates a correlation between MESTK and estrogen.2 However, rare cases were also reported in men and children.3 Even though malignant cases are rare, but they have also been reported for both genders. Since 2004, MESTK has been included in the World Health Organization renal tumor classification.
We report a 44-year-old Taiwanese male, with no history of hormonal therapy, who was found with a left renal tumor by self-health examination. Abdominal computed tomography showed an 11 x 15 cm enhanced heterogeneous soft tissue mass with calcification and minimal fatty content. He subsequently received radical left nephrectomy.
MESTK is a benign renal tumor with malignant potential. We should keep in mind that patients receiving hormonal therapy have a higher risk of developing cystic renal tumor, irrespective of their gender.
Manal M Thomas
National Research Centre, Egypt
Title: Genetic mutation in Egyptian children with steroid-resistant nephrotic syndrome

Biography:
Manal M Thomas is an Assistant Professor in Clinical Genetics department - Human Genetics and Genome Research division - National Research Centre, Cairo, Egypt. She has completed Master degree in Pediatrics from Medical School of Cairo University and PhD degree from Ain Shams University. She is a member of National Society of Human Genetics. She has many publications in medical genetics.
Abstract:
Nephrotic syndrome is the commonest etiology of proteinuria in children. Steroid-resistant nephrotic syndrome (SRNS) is defined by resistance to standard steroid therapy, and it continues to be one of the most intractable etiologies of renal failure. Molecular studies discovered specialized molecules in podocytes that play a role in proteinuria. Mutations in NPHS2 that encodes for podocin constitute a frequent cause of SRNS worldwide. This study aimed to screen for podocin mutations in SRNS Egyptian children and their parents. Our study included patients from 10 unrelated Egyptian families diagnosed with SRNS. Mutational analysis of the NPHS2 gene was performed by polymerase chain reaction amplification of the whole coding region of the gene and direct sequencing. Positive consanguinity was detected in five cases, and four of them had a positive family history of SRNS in a family member. Mutational analysis of NPHS2 revealed pathogenic mutations in four cases (40%) including a novel missense in one patient (c.1A>T; p.M1L). Our study concluded that mutations of NPHS2 gene are common among Egyptian children with SRNS. We support a model where ethnicity plays an important role in specific NPHS2 mutations, since a novel mutation was found in one patient in this study. Future study on a large number of Egyptian patients with SRNS is warranted to identify the actual genetic contribution of this gene in the development of SRNS in our population, which might help in patients’ prognosis and management.
